Professor Gordon Cook Clinical Director (Haematology) CTRU
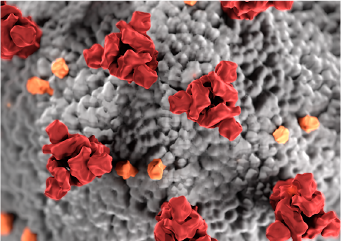
At the NIHR Leeds MIC, our cancer work focuses on blood cancer, looking at both diagnostics and informatics and in the first wave of the Covid-19 pandemic, I thought it was important that we registered the extent of the impact of COVID on patients with myeloma.
As a result, I started to generate a real time, real word, registry under the auspices of the UK Myeloma Forum. Here, on a voluntary basis, clinicians could log their myeloma patients, detailing laboratory and clinical parameters, including comorbidities and outcomes. It soon became apparent from this UK registry that myeloma patients were not doing as well as more general reporting indicated. As COVID evolved, the high risk groups were being delineated by age, ethnicity and comorbidities, but what our registry indicated was that myeloma seemed to have an uplift in mortality, even when taking these other factors into consideration. This uplift seemed to correspond with the immune disturbance that accompanies myeloma and associated treatments.
As I collected data from colleagues in Germany, other European countries, and North America and looked at that alongside the UK data, a global picture began to emerge, indicating that myeloma patients infected with COVID have a higher risk of mortality than any other cancer patients.
Working with colleagues at the Leeds MIC, I have developed a myeloma risk profile, using routine laboratory parameters and clinical trials which we published in 2019 . This has now been validated by real world data sets, both here and by colleagues abroad and is beginning to help us consider in more detail what host factors predispose myeloma patients in particular to a poorer outcome when they get COVID.
There was an overwhelming need from the NHS for guidelines on how to manage myeloma patients in the pandemic, which led to my contributions to the NICE guidelines, the National Transplant, and the UK Myeloma Forum guidelines. Focusing particularly on how to reduce hospital footfall, and recommending different approaches to treatments, or treatments that could be managed equally effectively remotely, or at home, these guidelines have now been adopted by the NHS.
Our early work identifying that myeloma patients are at a greater risk of mortality than any other immunocompromised patient group has been invaluable in informing the blood cancer work that I lead on the Octave diagnostic platform. This platform assesses vaccine response and has just received ethical approval to explore how myeloma patients will respond to the COVID vaccination. We already know that these patients generally respond poorly to the annual flu vaccination and the pneumonia vaccine, so we have an expectation that it is their poor immunity that makes myeloma patients more susceptible to COVID.
Myeloma is a rare cancer and, as such, was not on the government’s radar; our work had a significant impact in persuading the government that myeloma patients should be added to the list of high risk individuals who should be shielding.
Working with Myeloma UK, and involving patients as advocates, we presented data which resulted in myeloma patients being moved from cohort 7 or 8 up to cohort 4 on the government‘s shielding list . In turn, this research also played a significant part in ensuring that myeloma patients were a priority when considering how different groups respond to the COVID vaccine.
As we live through the science, our findings will continue to influence the treatment and management of myeloma patients at risk of infection, but these findings will also be significant, as we resume our research into myeloma diagnosis in the aftermath of COVID-19.
April 2021.
Further reading :
1. A Vijenthira, I Gong, T Fox, S Booth, G Cook, B Fattizzo, F M Moro, J Razanamahery, J Riches, J Zwicker, R Patell, M Vekemans, L Scarfo, T Chatzikonstantinou, H Yildiz, R Lattenist, I Mantzaris, W Wood & L Hicks. (2020) Outcomes of patients with hematologic malignancies and COVID-19: A systematic review and meta-analysis of 3377 patients. Blood doi.org/10.1182/blood.2020008824
2. A Chari, MK Samur, JM Lopez, G Cook, N Biran, K Yong, V Hungria, M Egelhardt, F Gay, A G Feria, S Oliva, R Oostvogels, A Gozzetti, C Rosenbaum, S Kumar, E Stadtmauer , H Einsele, M Beksac, K Weisel, KC Anderson, M-V Mateos, P Moreau, J San-Miguel, NC. Munshi &H Avet-Loiseau. (2020) Clinical Features Associated with SARS-CoV-2 Outcome in Multiple Myeloma: International Myeloma Society COVID-19 Registry Results. Blood, doi.org/10.1182/blood.2020008150
3. G Cook, AJ Ashcroft, G Pratt, R Popat, K Ramasamy, M Kaiser, M Jenner, S Henshaw, R Hall, J Sive, S Stern, M Streetly, C Bygrave, R Soutar, N Rabin & GH Jackson, on behalf of the United Kingdom Myeloma Forum. (2020) Real-world assessment of the clinical impact of symptomatic infection with severe acute respiratory syndrome coronavirus (COVID-19 disease) in patients with Multiple Myeloma receiving systemic anti-cancer therapy. British Journal of Haematology doi.org/10.1111/bjh.16874)
4. E Terpos, M Engelhardt, G Cook, F Gay, M-V Mateos, I Ntanasis-Stathopoulos, NWCJ van de Donk, H Avet-Loiseau, R Hajek, AJ Vangsted, H Ludwig, S Zweegman, P Moreau, H Einsele, M Boccadoro, J San Miguel, MA Dimopoulos & P Sonneveld. (2020) Management of patients with multiple myeloma in the era of COVID-19 pandemic: a consensus paper from the European Myeloma Network (EMN). Leukemia 22:1-12 doi.org/10.1038/s41375-020-0876-z